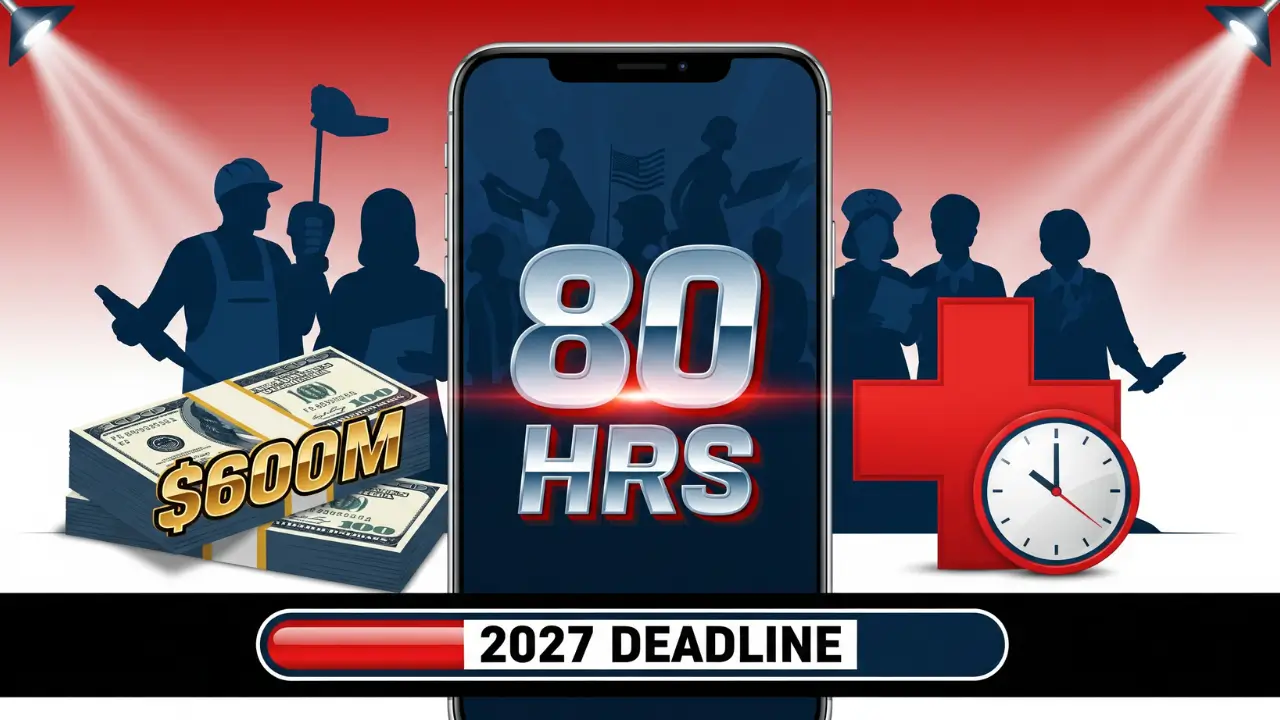
Ten major technology companies have pledged over $600 million in free and discounted services to help states enforce new Medicaid work requirements set to begin in 2027.
The announcement came from the Centers for Medicare & Medicaid Services (CMS) on January 29, 2026. It’s part of President Trump’s Working Families Tax Cut (WFTC) legislation, which now requires certain Medicaid recipients to work or participate in approved activities to keep their health coverage.
Starting January 1, 2027, adults on Medicaid must complete 80 hours per month of qualifying activities. These include employment, job training, education programs, or community service. States can choose to roll out the rules sooner if they’re ready.
The companies involved all have existing contracts with state Medicaid programs. They include Accenture, Conduent, Deloitte, Maximus, Optum, GDIT, and four others. Each firm is offering technology tools aimed at making the tracking process easier and cheaper for states.
Conduent is providing discounted system integration and offering its AI-driven fraud detection tool at no cost. Deloitte announced a discounted fixed fee per state for core system upgrades, along with a no-cost verification hub for the first year. Maximus will supply a Community Engagement Tracking Tool with mobile app and portal access at no development cost to current state clients.
GDIT plans to invest millions in an analytics platform to detect fraud, offering the base version free to states that sign service contracts. RedMane is discounting its AI tool called IntelliCoach, used to help SNAP agencies conduct client interviews, for $2 million per state per year.
CMS says the goal is to reduce the burden on both states and taxpayers while helping beneficiaries stay compliant. The technology will allow people to report work hours digitally, verify activities automatically, and connect to job resources in their area.
“This initiative represents a major reduction in implementation costs for states,” a CMS spokesperson said in a press release. The $600 million figure reflects the total value of donated and discounted products being offered across all ten companies.
Federal law now mandates these requirements, and the HHS Secretary must issue an interim final rule by June 1, 2026. States are expected to begin preparation immediately, even if full enforcement doesn’t begin until 2027.
Advocates worry the changes could lead to coverage loss for vulnerable adults who are unable to meet the monthly activity threshold. Others argue the requirements will encourage workforce participation and reduce improper enrollment.
More guidance is expected in the coming months. States and the public can find updates on Medicaid.gov and through official fact sheets from CMS.
For now, millions of Medicaid recipients should prepare for major changes ahead.